Introduction to Atrial Fibrillation in the Elderly
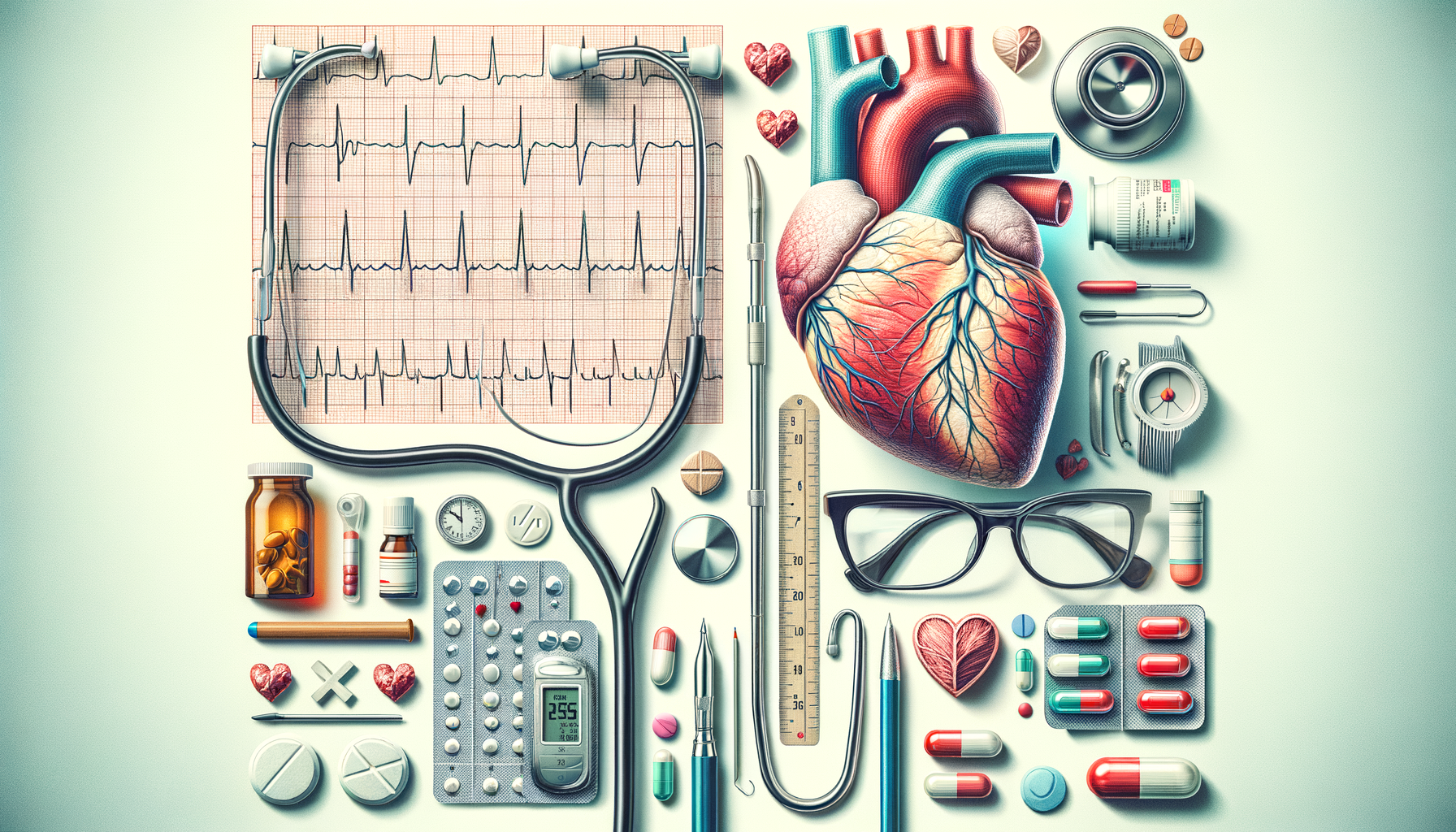
Atrial fibrillation (AFib) is a common heart rhythm disorder that becomes increasingly prevalent with age. It is characterized by an irregular and often rapid heart rate that can lead to various complications, including stroke and heart failure. The elderly population is particularly susceptible to AFib due to age-related changes in heart structure and function. Understanding the specific challenges and considerations for treating AFib in older adults is crucial for ensuring effective management and improving quality of life.
Managing AFib in the elderly requires a comprehensive approach that balances the benefits and risks of treatment options. The goal is to control the heart rate, restore normal rhythm, prevent blood clots, and address any underlying conditions contributing to AFib. Given the increased risk of complications in older adults, personalized treatment plans are essential to address individual health needs and preferences.
Medication Management for AFib in Older Adults
Medication is often the first line of treatment for managing AFib in older adults. Anticoagulants are commonly prescribed to reduce the risk of stroke by preventing blood clots. However, the use of anticoagulants in the elderly requires careful consideration due to the increased risk of bleeding. It is vital to assess the patient’s overall health, kidney function, and potential interactions with other medications before prescribing anticoagulants.
Rate control medications, such as beta-blockers and calcium channel blockers, are used to manage the heart rate. These medications help reduce symptoms such as palpitations and fatigue, improving the patient’s quality of life. Rhythm control medications, also known as antiarrhythmics, aim to restore and maintain a normal heart rhythm. However, these drugs may not be suitable for all elderly patients due to potential side effects and interactions.
In some cases, a combination of rate and rhythm control medications may be necessary to achieve optimal results. Regular monitoring and follow-up appointments are essential to ensure the effectiveness of the treatment and to make any necessary adjustments.
Non-Pharmacological Treatments for AFib
In addition to medication, non-pharmacological treatments play a vital role in managing AFib in older adults. Lifestyle modifications, such as maintaining a healthy diet, regular physical activity, and avoiding excessive alcohol and caffeine, can significantly impact AFib management. These changes help improve overall cardiovascular health and may reduce the frequency and severity of AFib episodes.
Catheter ablation is a minimally invasive procedure that can be effective for patients who do not respond well to medications. This procedure involves using radiofrequency energy to destroy the small areas of heart tissue responsible for the irregular rhythm. While catheter ablation can be highly effective, it is not suitable for all elderly patients, particularly those with other significant health issues.
Another option is the use of pacemakers, which can help regulate heart rhythm in certain cases. Pacemakers are particularly useful for patients with bradycardia, a condition characterized by a slow heart rate. The decision to use a pacemaker or undergo catheter ablation should be made in consultation with a cardiologist, taking into account the patient’s overall health and treatment goals.
Risk Assessment and Monitoring
Regular monitoring and risk assessment are essential components of AFib management in older adults. Healthcare providers should conduct thorough evaluations to identify potential risk factors, such as hypertension, diabetes, and sleep apnea, which can exacerbate AFib symptoms. Monitoring tools, including Holter monitors and event recorders, can help track heart rhythm patterns and guide treatment decisions.
Risk assessment tools, such as the CHA2DS2-VASc score, are used to evaluate the risk of stroke in patients with AFib. This score considers factors such as age, gender, and the presence of other medical conditions to determine the need for anticoagulation therapy. Regular follow-up appointments are crucial for adjusting treatment plans and addressing any new or worsening symptoms.
Patient education is also a key component of risk management. Educating patients and their families about the signs and symptoms of AFib, potential complications, and the importance of adherence to treatment plans can empower them to take an active role in their healthcare.
Conclusion: Tailoring Treatment for Optimal Outcomes
Treating atrial fibrillation in older adults requires a thoughtful and individualized approach. By considering the unique needs and health conditions of elderly patients, healthcare providers can develop effective treatment plans that prioritize both heart health and overall well-being. The combination of medication, non-pharmacological treatments, and regular monitoring can help manage AFib symptoms and reduce the risk of complications.
Ultimately, the goal is to improve the quality of life for older adults living with AFib. With advances in medical treatments and a better understanding of the condition, effective management is within reach. By working closely with healthcare providers, patients and their families can navigate the complexities of AFib treatment and achieve optimal outcomes.