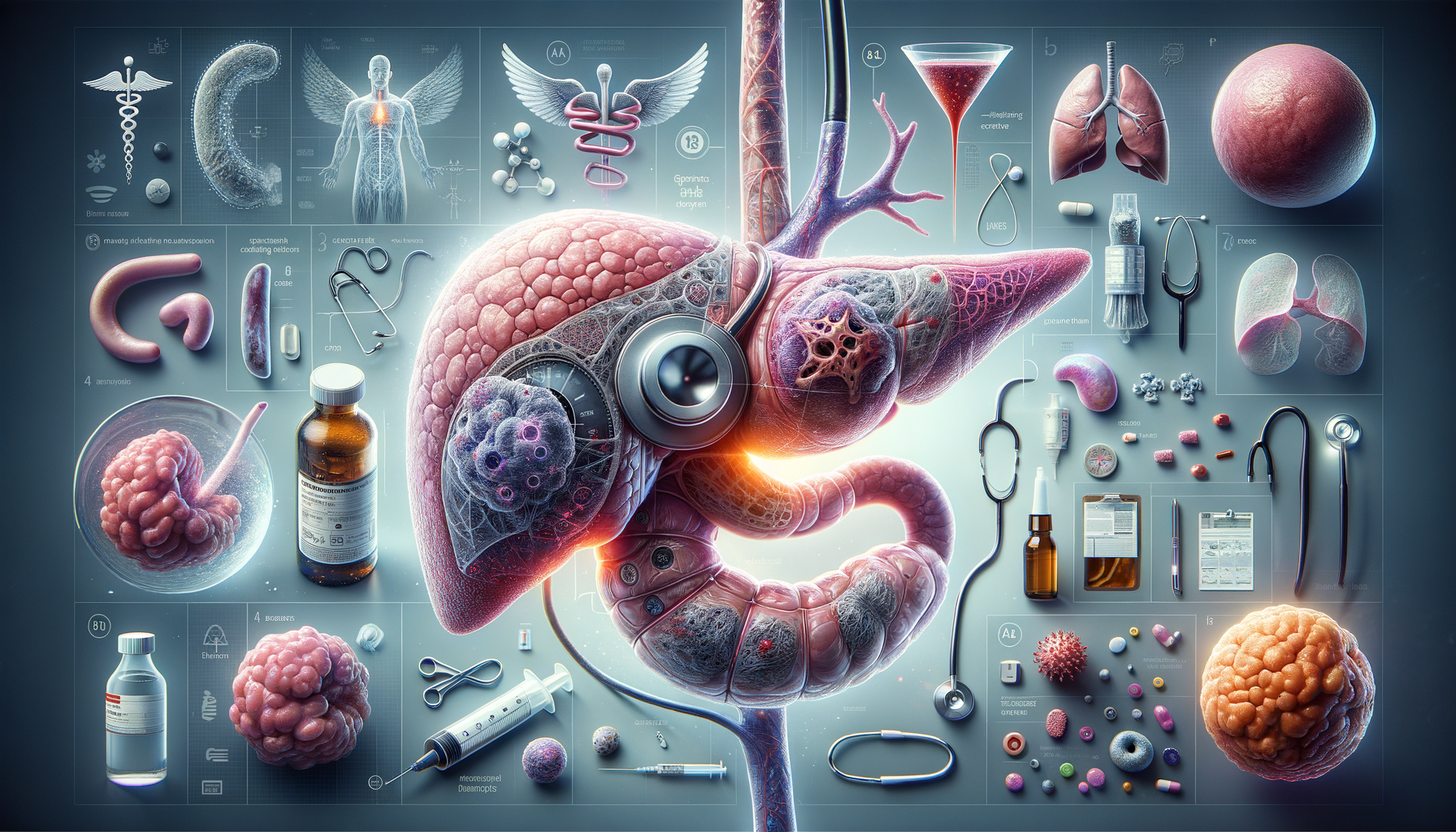
Introduction to Pancreatic Cancer
Pancreatic cancer is a formidable disease that presents unique challenges in diagnosis and treatment. Located deep within the abdomen, the pancreas plays a crucial role in digestion and blood sugar regulation. When cancer develops in this organ, it often progresses silently, making early detection difficult. Understanding the nature of pancreatic cancer is essential for improving patient outcomes and advancing research efforts.
The pancreas, a small organ nestled behind the stomach, is responsible for producing enzymes that aid in digestion and hormones like insulin that regulate blood sugar levels. Pancreatic cancer occurs when cells in the pancreas grow uncontrollably, forming a tumor. This type of cancer is notorious for its aggressive nature and poor prognosis, often because it is diagnosed at an advanced stage.
Raising awareness about pancreatic cancer is vital, as it remains one of the leading causes of cancer-related deaths worldwide. Efforts to improve early detection, treatment options, and patient support are ongoing, with researchers and healthcare professionals striving to make significant strides in combating this disease.
Risk Factors and Causes
Understanding the risk factors associated with pancreatic cancer is crucial for prevention and early detection. While the exact cause of pancreatic cancer is not fully understood, several factors have been identified that may increase an individual’s risk.
Some of the known risk factors include:
- Age: The risk of developing pancreatic cancer increases with age, with most cases occurring in individuals over 60.
- Smoking: Tobacco use is a significant risk factor, with smokers having a higher likelihood of developing pancreatic cancer compared to non-smokers.
- Family history: A family history of pancreatic cancer or certain genetic syndromes can increase risk.
- Obesity: Being overweight is linked to an increased risk of developing pancreatic cancer.
- Chronic pancreatitis: Long-term inflammation of the pancreas is associated with a higher risk.
While these factors can contribute to the development of pancreatic cancer, it is important to note that having one or more risk factors does not guarantee that a person will develop the disease. Conversely, some individuals with pancreatic cancer may not have any known risk factors. Ongoing research aims to uncover more about the genetic and environmental influences on pancreatic cancer development.
Symptoms and Diagnosis
Pancreatic cancer is often called a “silent” disease because it typically does not cause symptoms in its early stages. By the time symptoms appear, the cancer may have already advanced. Recognizing the symptoms and seeking medical attention promptly can be crucial for diagnosis and treatment.
Common symptoms of pancreatic cancer include:
- Jaundice: A yellowing of the skin and eyes, often accompanied by dark urine and pale stools.
- Abdominal pain: Pain or discomfort in the upper abdomen or back.
- Weight loss: Unintentional weight loss and loss of appetite.
- Nausea and vomiting: Digestive issues that may include nausea and vomiting.
- New-onset diabetes: Sudden onset of diabetes in individuals without risk factors.
Diagnosing pancreatic cancer typically involves a combination of imaging tests, such as CT scans or MRIs, and biopsy procedures to examine tissue samples. Blood tests may also be used to detect tumor markers. Due to the complexity of the disease, a multidisciplinary approach involving oncologists, radiologists, and pathologists is often necessary to confirm a diagnosis and determine the best course of treatment.
Treatment Options
Treating pancreatic cancer requires a comprehensive approach tailored to the individual patient’s needs. The choice of treatment depends on several factors, including the stage of the cancer, the patient’s overall health, and the tumor’s location.
The primary treatment options for pancreatic cancer include:
- Surgery: Surgical removal of the tumor is the most effective treatment for early-stage pancreatic cancer. Procedures such as the Whipple procedure may be performed to remove the tumor and surrounding tissues.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells or stop them from growing. It may be used before or after surgery, or as the main treatment for advanced cancer.
- Radiation therapy: High-energy rays are used to target and destroy cancer cells. Radiation therapy may be combined with chemotherapy to enhance effectiveness.
- Targeted therapy: This treatment uses drugs that target specific molecules involved in cancer cell growth and spread.
- Immunotherapy: A newer approach that helps the body’s immune system recognize and attack cancer cells.
While these treatments can be effective, pancreatic cancer remains challenging to treat due to its aggressive nature and tendency to spread quickly. Clinical trials and research are ongoing to develop new therapies and improve existing ones, offering hope for better outcomes in the future.
Living with Pancreatic Cancer
Receiving a diagnosis of pancreatic cancer can be overwhelming, but support and resources are available to help patients and their families navigate this difficult journey. Living with pancreatic cancer involves managing symptoms, undergoing treatment, and addressing the emotional and psychological impact of the disease.
Supportive care is an essential component of living with pancreatic cancer. This includes:
- Pain management: Effective pain control is crucial for maintaining quality of life.
- Nutritional support: Maintaining proper nutrition can be challenging, but it is vital for strength and recovery.
- Emotional support: Counseling, support groups, and mental health services can help patients cope with the emotional challenges of cancer.
- Palliative care: Focuses on relieving symptoms and improving quality of life, regardless of the stage of the disease.
Patients are encouraged to communicate openly with their healthcare team to address any concerns and explore all available options. Advances in treatment and supportive care continue to improve the outlook for those living with pancreatic cancer, providing hope and better quality of life.